Injuries and fractures
4 The value of the use of physiotherapy for fractures
General information
Leg fractures are an extremely common injury, accounting for 45% of total skeletal injuries.
A leg fracture can be isolated or multiple, or it can be observed as part of a concomitant injury.
The severity, timing and methods of treatment, as well as long-term effects can vary significantly depending on the level and characteristics of the fracture. Common signs of leg fractures are swelling, pain, and impaired support and movement. Pathological mobility and crepitus are often detected. To clarify the diagnosis, radiography and CT are used, in some cases MRI and arthroscopy are prescribed. Perhaps both conservative and surgical treatment.
Fracture classification
Leg fractures can be complete or incomplete (fractures). Fractures of the legs that communicate with the external environment through a wound on the skin are called open. If there is no wound, the fracture is closed.
Depending on the features of the fracture line and the nature of the fragments, the following types of leg fractures are distinguished in traumatology:
- Transverse - the fracture line is located transversely to the length of the bone.
- Oblique - the fracture line is at an angle to the length of the bone.
- Longitudinal - the fracture line is located along the length of the bone.
- Helical - the fracture line has a spiral shape (such injuries are usually formed as a result of a sharp violent twisting of the limb).
- Polyfocal - there are two or more large bone fragments.
- Fragmented - there are several fragments.
- Shattered - there are many small fragments.
- Compression - accompanied by compression of the bone. In this case, the bone cracks, flattens, squeezes and deforms.
- Impacted - accompanied by the introduction of one fragment into another.
- Avulsion - a small fragment breaks off from the bone (for example, when a ligament is torn off at the place of its attachment).
Taking into account the level of the leg fracture, there are:
- Fractures of the femur;
- Fractures of the bones of the lower leg;
- Fractures of the bones of the foot.
Injuries to the proximal and distal ends of the bone can be intraarticular (epiphyseal) or periarticular (metaphyseal). With intra-articular leg fractures, concomitant damage to various articular structures, including cartilage, capsule and ligaments, is observed. Perhaps a combination with subluxation or dislocation.
Fracture healing
After a fracture, the body immediately tries to restore the bone tissue to its original state. It takes six weeks to several months for the bone to heal completely.
Immediately after the fracture, bleeding begins from the damaged vessels of the periosteum (Fig. 1). A blood clot called a hematoma forms. The blood coagulates, stops flowing out, and fibrous connective tissue gradually forms in place of its clot. After a few days, tough tissue called calluses develops at the sites of the hematoma. Cells called fibroblasts begin to produce fibers of collagen, the main protein in bone and connective tissue. Chondroblasts then begin to produce fibrous cartilage. This tissue stiffens calluses by closing the gap between parts of the bones. This process takes about three weeks.
Callus after a fracture. Next, osteoblasts begin to produce bone cells, turning calluses into calluses. This bone shell provides the necessary protection for 3-4 months before the bone goes through the final stage of healing.
A sufficiently large amount of time must elapse before the bone is ready to take on the full load. Osteoclasts and osteoblasts will work for several months to turn the callus into a full-fledged bone tissue. These cells also reduce the bulge, returning the bones to their original appearance. Circulation improves along with an influx of nutrients such as calcium and phosphorus, which strengthen bones.
Even the most minor fractures require medical attention so that the healing process goes as quickly as possible.
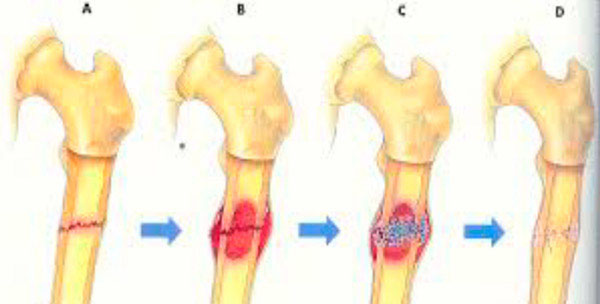
Fig.1
The value of the use of physiotherapy for fractures
After a fracture, you must first restore the integrity of the damaged bone. For this purpose, methods of traction, immobilization and surgical intervention are used.
But no less important is the return of mobility, innervation, trophism of the injured limb. Medicine has many methods aimed at rehabilitation after fractures, and one of the most significant is physiotherapy.
It is difficult to overestimate the importance of physiotherapeutic procedures at the stages of treatment and rehabilitation after fractures. As part of complex therapy, they contribute to recovery and return to working capacity, alleviate the patient's condition. The main tasks of physiotherapy treatment:
- prevention of muscle atrophy and the formation of contractures;
- reduction of puffiness;
- elimination of pain syndrome;
- improvement of microcirculation and tissue nutrition;
- prevention of infectious and inflammatory processes in open fractures.
A properly selected set of procedures not only promotes recovery, but also reduces the drug load on the body.
The choice of specific methods of physiotherapy treatment directly depends on the stage of bone tissue regeneration.
The following types of physiotherapy are shown: UHF, MAGNETOTHERAPY, ELECTROPHORESIS, MASSAGE, LYAPKO APPLICATION THERAPY, ETC.
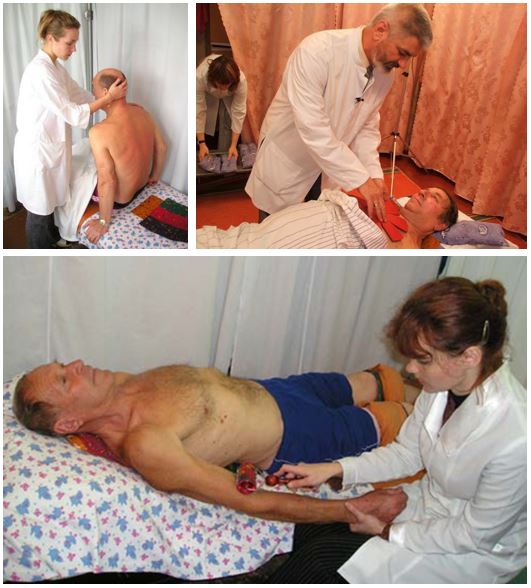
Application therapy Lyapko
Lyapko's applicators in various modifications (plates, rollers, applique belts, applique tapes) are an original, powerful device with many health-improving therapeutic possibilities. Their action is based on the principles of traditional Chinese medicine - superficial multi-needle acupuncture, as well as on the general physiological mechanisms of life.

Mechanisms of action of the applicator
The high healing effect of Lyapko applicators is due to a combination of intense reactions:
- reflex-mechanical;
- galvano-electric;
- immunological.
The clinical effects of the method of multi-needle therapy are manifested in analgesic, antispasmodic, anti-inflammatory, anti-edematous, neurotrophic and immunomodulatory effects. Also in the regulation of the functions of the autonomic nervous system, the normalization of the processes of excitation and inhibition in the central nervous system.
Application therapy for injuries and fractures of the lower extremities, fracture of the femoral neck.
If there are metal plates, pins, fragments in the patient's body, then any type of electrophysiotherapy is contraindicated for them and the only means of physiotherapeutic treatment is the Lyapko applicator. Lyapko's application therapy can be used from the first days of an injury or fracture, it is combined with all types of medical and physiotherapeutic treatment.
How to work with the applicator, application zones
In 90% of cases, it is necessary to act on the pain zone, and to increase efficiency on additional and auxiliary zones. It is always necessary to include the main zone (the region of the spine) in the general recipe.
Additional and auxiliary zones should be used when, for a number of reasons, it is impossible to influence the main zone (gypsum is applied, the wound surface). To enhance the therapeutic effect, it is advisable to include in the formulation the effect on the symmetrical zones of the healthy side.
The main zones are located on the back surface of the trunk, head, neck.
The main ones are named due to the fact that the skin areas on both sides of the spine and directly above the spine are closest to the exits of the roots of the cranial and spinal nerves and other structures.
Auxiliary zones: front surface of the trunk, head and neck.
Additional zones: zones of the skin of the lower and upper extremities, which are secondary (peripheral) in relation to the (central) structures of the spinal cord and brain.
General recommendations
In the old days, healers, in the treatment of fractures, practiced this method: with a small file from an old copper coin, copper powder was planed. A little of this powder (1/10 gram), stirred in milk or sour cream, or rubbed with egg yolk and given to the patient inside, 2 times a week. This accelerated the healing of fractures.
You need to eat food rich in vitamins and microelements such as: manganese, copper, zinc, phosphorus, calcium, magnesium, vitamins B6, B9, B12, C, D, K. All these elements help to absorb calcium and protein - from which the body and will build bone tissue.
It is advisable to use the mummy inside and outside (in solution) on the fracture area.
In the early days, with pathology of muscles, bones and joints, rest should be observed, but in the future, physical activity should be gradually increased. If the muscles do not work, they quickly weaken and atrophy. Without load, the work of the ligamentous-articular apparatus is disrupted, which lengthens the process of recovery and recovery after an injury, and increases the likelihood of future injuries.
After the cast is removed, the muscles are always painfully tense, require gradual stretching, and the joints need to be “developed”. After removal of the plaster, pain can appear in almost all parts of the back, since immobilization of both the upper and lower limbs after fractures leads to a gross violation of the stereotype of movements of the whole body and the appearance of pronounced asymmetries of the body.
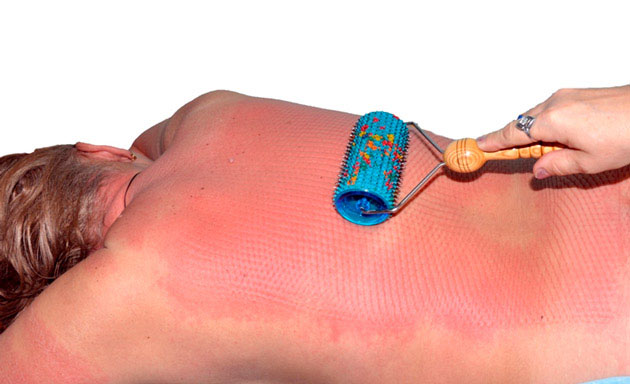
Therefore, to prevent the appearance of muscle pain in the back, from the first days of the fracture, flat applicators should be applied to the back for 20-30 minutes in the evening, roll the back with the "Big Roller M" , "Universal Roller M" in the morning and afternoon for 3-5 minutes (until a uniform pink color appears). Do a back massage using the Pharaoh massager .
 |
 |
When applying plaster in the first days, there is often a strong swelling, increased pain at the fracture site, leading to the fact that the plaster has to be incised.
First of all, you need to act with any flat applicators: “Chamomile M” , “Insoles Plus” , “Quadro” , “Chance” on the lumbosacral zone of the spine, from where the innervation to the limb comes from - the main zone, if there is access there.
Then it is recommended to act on all free surfaces of the legs above and below the fracture site (plaster cast), as well as on a healthy leg, focusing on the symmetrical fracture site, this reflexively reduces swelling and pain on the injured limb. The impact can be carried out both with a flat applicator and with a roller. Also, you can use static-dynamic applicators: “Magic tape “Health”, belt “Universal M”, belt “Baby”. They need to be fixed on the limb for a longer time from 30 to 60 minutes 2-3 times a day.
For injuries - the same technique. If the skin over the injured area of the limb is not damaged, then you can act on the site of injury. In case of bruises, to avoid the occurrence of edema, hematomas, you can fix any flat applicator, application tape or roll it with a roller to this place.
Application zones (Fig. 2): main 7.8; additional 18; auxiliary 26, 28, 30, (22, 27, 29).
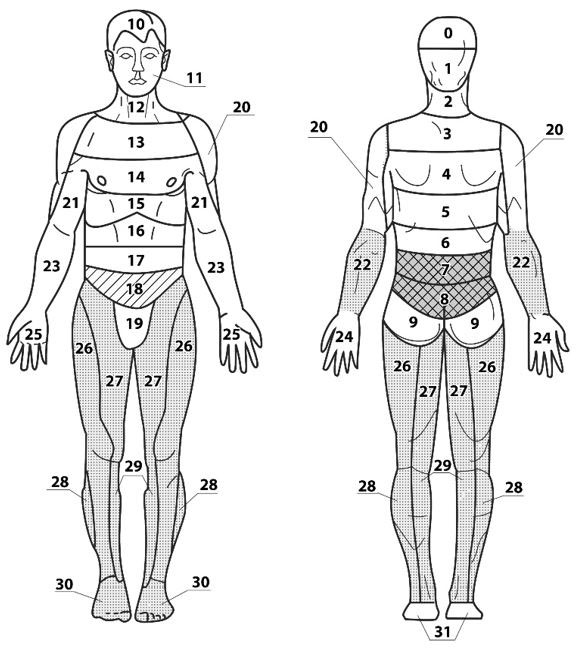
Fig.2
Work on the feet with applique insoles or roll them with the “Large Roller M” , “Universal Roller M” .

The duration of exposure on the side of the fracture is 2 times longer than on the healthy leg. For example, we act for 15-20 minutes with static applicators on the lumbosacral zone and on the sore leg, symmetrically - on the healthy leg for 5-7 minutes. The same technique for injuries.

Additional recommendations. A good result gives a short-term effect on the symmetrical zones of a healthy limb, the zones of correspondence on the hands and feet, used in Su Jok therapy (Fig. 3)
You can roll with "Needle Ball" , "Large Roller M" , "Universal Roller M" , "Face Roller M" , also make squeezes with the Kraplinka applicator .
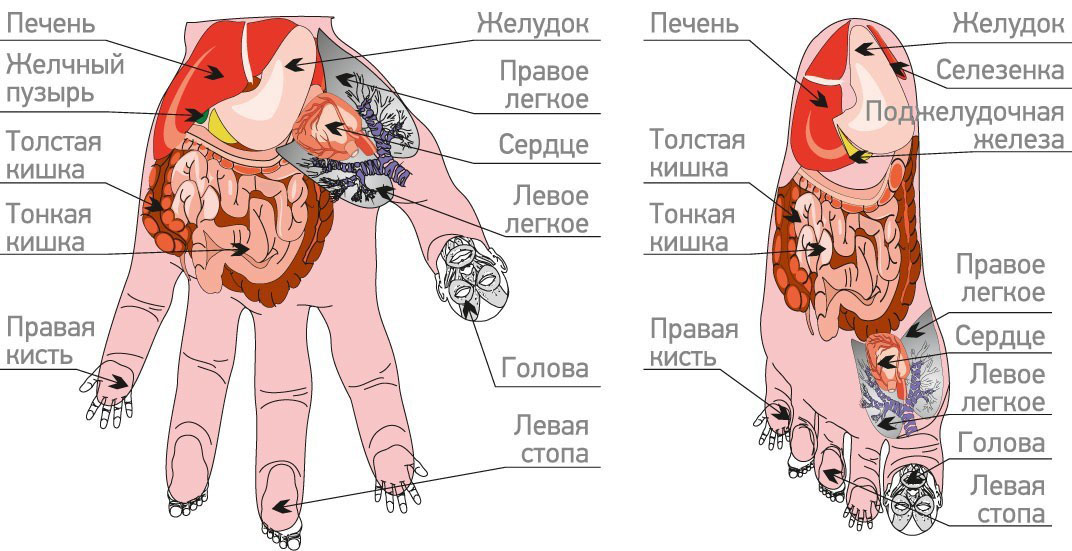
Fig.3
Recommendations for the selection of crutches
The choice of crutches should be approached very responsibly, since crutches that are incorrectly selected for height can cause various lesions of muscle, bone tissue and nerves (inflammation of the shoulder joint, traumatic plexitis, etc.). Low crutches lead to excessive stoop, the use of one crutch leads to lateral curvature of the spine.

Hip fractures
Fractures of the femoral neck are intra-articular, more often occur in older patients suffering from osteoporosis.
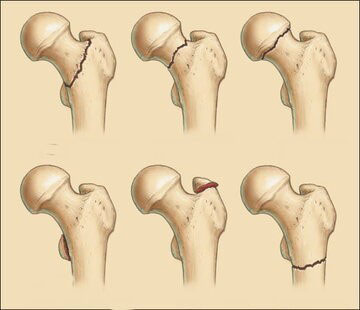
A broken leg occurs as a result of a fall at home or on the street. With a decrease in bone strength, its integrity can be violated even when turning the body in bed.
Due to insufficient blood supply, the femoral neck does not heal well, a full-fledged callus, as a rule, is not formed, the fragments are “grasped” together by the connective tissue, which leads to a high percentage of disability. Given this circumstance, the preferred method of treatment for such leg fractures is surgery - osteosynthesis with a three-blade nail, arthroplasty or bone autoplasty.
If the general condition does not allow for surgical intervention, skeletal traction is used. Patients of senile age impose a plaster boot with a transverse bar, excluding the rotation of the limb. This allows for the formation of fibrous callus while maintaining sufficient physical activity of the patient.
With fractures of the femoral neck, after surgical treatment on the hip joint, application therapy is used as measures aimed at developing the joint, improving blood supply, increasing muscle tone, and helping to get out of a depressive state.
It is recommended to roll a healthy, sore leg with a roller, laying flat applicators of large sizes on a sick and healthy leg, on the lumbosacral zone and the buttocks zone.

The use of applicators on the back, on the chest area in front is a means of preventing pulmonary congestion, which can lead to pneumonia and death of the patient.
For many elderly patients, such procedures have helped to avoid these complications and return to normal life.
